It sounded like a weapon out of “Guardians of the Galaxy”
– Paul Raeburn, Writer in MedPage Today (2017)
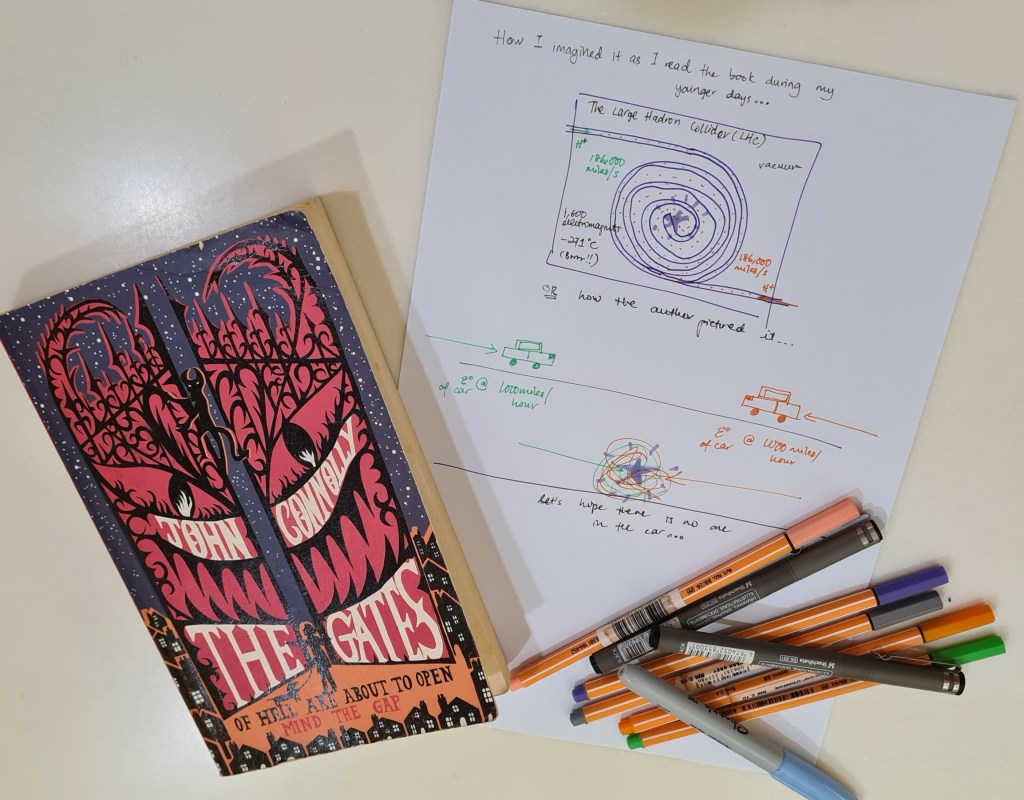
When I first read about particle colliders in a book by John Connolly, ‘The Gates’, it was about how the fate of humanity lies in the hands of “one small boy, an even smaller dog, and a very unlucky demon named Nurd”. An in there, the author explained about the Large Hadron Collider and how beams of hydrogen ions were being whizzed around before colliding inside this ring-shaped tunnel at CERN*. To put it into layman’s perspective, the author decided to use cars as an example – imagine the energy of a big car travelling at 1000 miles/hour…and crashing into another car travelling at that same speed (not good!). A rather unconventional work of fiction in the palm of your hands, really.
So what does the demon, the dog and the small boy got to do with this scientific jargon? – well I guess you gotta read the book yourself. It comes highly recommended! 🙂
I’ve always found particle accelerators intriguing, and having read a lot of fictional storybooks as a child, I was curious as to how big these contraptions were in real life.
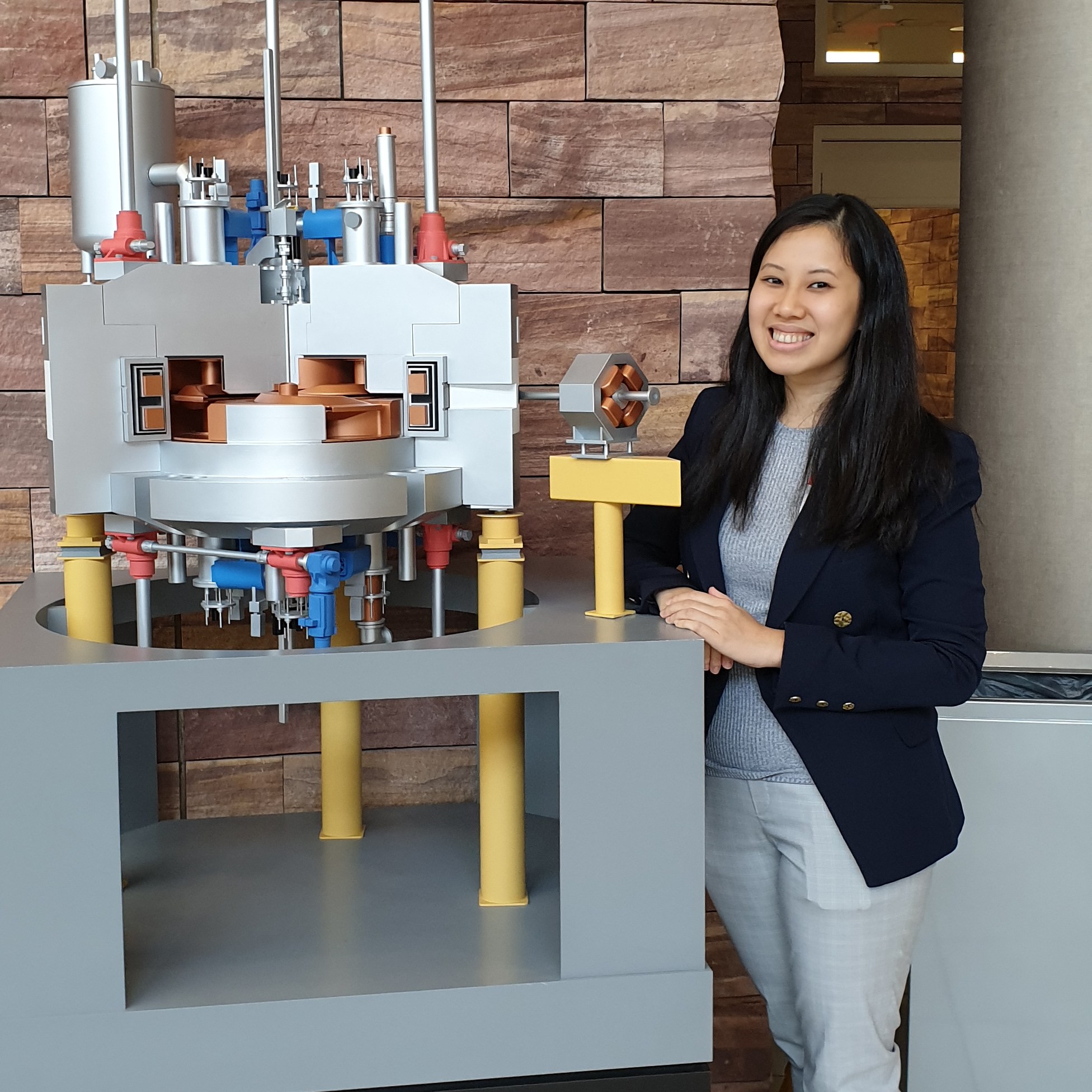
Well, I have never been to CERN* (the European Organization of Nuclear Research), if that is what you had in mind, but seeing a proton machine up close made me realise how gigantic these structures were. In my current role, I was very fortunate to have had the opportunity to visit a Proton Therapy site in California during one of my on-the-job training attachments. Before delving deeper into my clinical experience at the California Protons Cancer Therapy Center in San Diego, here is a brief introduction to proton therapy…
What is proton therapy?
Just to shed some light (if you are reading this as a layman or a medical professional) – proton therapy or proton beam therapy is a type of radiation therapy which uses proton particles instead of X-rays to treat cancer. A synchrotron or cyclotron is the machine that accelerates the proton particles to an extremely high speed, thus creating a high energy flux. It is this energy that makes protons travel to the desired depth in the body.
So…why Protons?
These positively charged particles, protons, are accelerated to more than ¾ the speed of light and are targeted at the tumour tissue. Due to the nature of these particles and their behavior unlike conventional X-rays, protons dissipate all of their energy into the target thus leaving less radiation dose outside of the tumour. Depending on the speed and energy, these ions can reach up to 30 centimetres deep into the tissue. However, X-rays, do not. They would lose a large part of their energy to the surrounding tissues on the way to the tumour and continue to leave a trail of radiation even after passing the tumour; thus possibly causing side effects to neighbouring healthy cells.
See some of my sketches below to get a pictorial explanation of protons vs photons (X-rays).

The Investment needed for a Proton Therapy Centre
If you are curious about how much these proton therapy centres and their treatments typically cost, an article by Bryant Furlow on “Cost vs Benefits: The Controversy Over Proton Beam Radiotherapy” pretty much sums it up. From an excerpt in the article, “Depending on the number of rooms and other factors, these facilities can cost more than $225 million each and have been called the single most expensive medical device ever built. Perhaps not surprisingly, treatment costs exceed those of traditional photon external-beam radiotherapy (EBRT) modalities.”
As a better form of comparison, proton therapy costs range from about $30,000 to $120,000. In contrast, a course of treatment with radiosurgery (X-rays) costs about $8,000 to $12,000. A radiation treatment center with stereotactic capabilities costs about $7 million to build, versus roughly $200 million for a proton therapy center. (Source: Dwight Heron, MD, chairman of radiation oncology at UPMC Shadyside in Pittsburgh)
“But proton therapy’s allure is strong despite its costs.”
– Bryant Furlow on “Cost vs Benefits: The Controversy Over Proton Beam Radiotherapy“

A visit to the California Protons Cancer Therapy Center, San Diego
Apart from everything being larger than life, everything from how protons interact with matter (tissue) to its treatment planning and also daily delivery were new concepts for me to grasp and understand.

Fortunately for me, the team at the California Protons Centre were just AMAZING! Walking into the naturally lit, open space of the cancer centre’s lobby that was both beautiful but a tad overwhelming kind of made me feel like a patient walking in for treatment for the very first time. Although it was clean, bright, a tastefully decorated; just the thought of not knowing what to expect was that overwhelming bit for me! But everyone, from the doctors, to the radiation staff and administrators were warm and welcoming; and that definitely made my learning experience a very memorable one.
After the introductions and site tour, I was stationed at CT simulation before moving on to treatment planning and finally the treatment rooms, so that I could understand the entire workflow better.
CT-Simulation for Proton Therapy
Patient simulation procedures were especially challenging, where density is one of the main concerns in proton treatment planning. Therefore, imagine treating areas where density would be a problem, like fluctuations in the daily volume of the bladder or rectum or even treatment of tumours in the lung! However, one thing that stood out to me as a Radiation Therapist working with photons (X-rays), is the attention to detail when it comes to patient setup and immobilization in Proton Therapy.
A radiation therapist performing CT-simulation for patients undergoing proton therapy will also need to carefully consider the patients’ immobilization pose, and the expected treatment beams that will be used for the type of cancer. Masks, vacuum bags or moulds should then be fabricated after considering all these aspects. Typically, the radiation therapist will also inspect the immobilization devices for wrinkles, folds, etc. that may introduce problematic heterogeneities (inconsistencies) during treatment planning.
Also, another concept unique to proton simulation and planning is that the patient has to be scanned with the couch top and all immobilization devices in the scanned images, if possible. All of these will be contoured accordingly and included as the ‘BODY’ should the immobilization device be in the proton beam line.
On top of that, internal immobilization is also adopted in proton therapy. Devices such as fiducial markers, endo-rectal balloons or rectal spacers are used inside the patient to localize or regulate internal anatomy position. However, density of these markers should always be taken into careful consideration as they may pose unique challenges in proton therapy such as creating CT artifacts and dose shadows.
Endo-rectal balloons are also more commonly adopted in prostate proton therapy as it helps to reduce inter- and intra-fractional variation of the prostate position within the body and also limiting the volume of the rectal wall within the high dose treatment area. In proton clinics, these balloons are usually filled with water! This is to avoid gas pockets and heterogeneities along the path of the lateral beams.
Proton Treatment Planning (from a Radiation Therapist perspective)
Due to the unique properties of proton beams, proton treatment planning exhibit very steep dose gradients and transition from full dose to zero dose very quickly. Also, the plans are extremely susceptible to deterioration if there’s any interference between the proton beam and the immobilization device. Therefore, it is critical to ensure robust and reliable immobilization for each patient.
Protons when travelling through sharp edges of the treatment couch or across the rough corners of vacuum bags will ‘bend the beam’ (shifted range) from the original plan. Now imagine if there is a critical structure lying close to the area that you are targeting and the new ‘shifted’ beam deposits all its dose there instead!
But of course, there is so much more to proton planning and this is just barely scraping the surface.
Proton Treatment

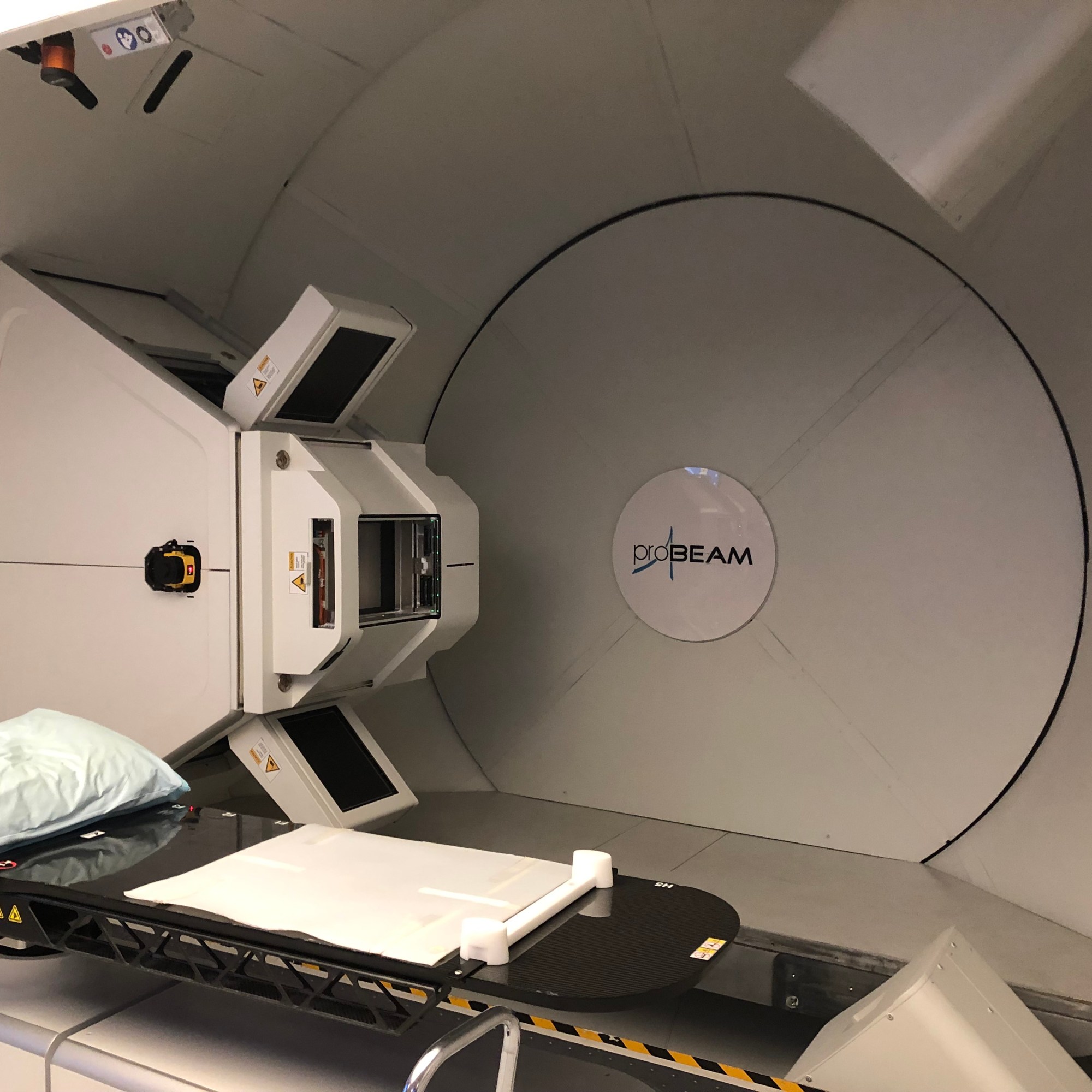
At California Protons, three gantries (treatment rooms) were used to treat patients and the site saw a majority of prostate cases, breast treatments, pediatric and neurological cases as well.
Each daily treatment began with a detailed imaging process to ensure that the radiation was delivered to the precise treatment location. As the team at California Protons were one of the early adopters of the Varian ProBeam proton technology, they had developed local imaging protocols catered to their patient base and treatment techniques.
During my observation of the treatment rooms, I was amazed at how each group worked so well with those from other treatment rooms (they were all separated to their own treatment rooms so they could not see one another!). The team had figured a way of optimizing their workflow for patient throughput, while maintaining reasonable patient wait times – and it all worked seamlessly like clockwork! The smooth, ‘uninterrupted’ workflow was to ensure that the cyclotron was being utilized at its best capacity – otherwise, patient wait time and machine idle time may be disrupted.
Although it was a short observational visit, it definitely gave me a good insight into the world of proton therapy. Perhaps, if given the opportunity in the future, this is one avenue that I definitely want to explore and understand more!
I would also like to take this opportunity to thank the amazing team at California Protons. You know who you are and I am definitely missing you all!
Author’s note: This was the author’s first experience with proton therapy and the author has never used the technology clinically or handled patients undergoing proton treatment. The observational visit was purely for educational purposes and the experiences documented here are solely the author’s own.




So glad you got such excellent exposure opportunities.
LikeLiked by 1 person