Author’s Note: Name(s) and examples used for the purpose of this 3-section blog post are entirely fictional and any coincidental representations are not intended. Opinions are the author’s own and must not be misconstrued as guidelines or medical advice.
It is today.
Another date that Auntie Jen would most likely remember for the rest of her life.
A prolific lawyer with many accolades, Auntie Jen hardly ever took a break off work. She always felt that she could never quite find enough time to counsel the volume of clients that needed her aid.
But today, today – clients can wait. Work can wait.
Dark clouds hang ominously in the sky and streaks of lightning zig-zagged forebodingly across the heavens. An audible roll of thunder can be heard; signaling that a storm was near.
As Auntie Jen pulls her brand-new red sedan into the already packed Cancer Centre parking lot on an early Monday morning, the first few drops of rain lands loudly on her windshield.
“Breathe, breathe, breathe.”

It has been a few weeks since her consultation with Dr Culler and post that, a series of other appointments ensued. In the most recent consultation, Auntie Jen was referred and introduced to Dr Culler’s colleague – a bright and bubbly Radiation Oncologist1 (a doctor specializing in giving radiation therapy to treat cancer) who goes by the name of Dr Wong.

After Auntie Jen’s initial consultation with Dr Wong, she has been given an appointment for her CT-Simulation procedure at the Radiation Oncology department. Dr Wong had explained to Auntie Jen that the CT-Simulation process is required in order for the team to “map” out and define the exact location of the cancer to be treated.
Therefore, in order to accomplish this, Dr Wong’s team of Radiation Therapists2 (an Allied Health Professional who uses radiation therapy to treat cancer) will be using a CT-scan machine at the department to acquire the images of Auntie Jen’s treatment area that will be used for the planning process moving forward.
Making her way to the patient registration counter, Auntie Jen couldn’t help but notice the sound of her heart beating louder against her chest with every step she takes. The registration had been swift. Shortly after, the clinic assistant ushers her to a seat by the window in the patient waiting area.

By then, the clouds had cleared, giving room to a hint of sunshine to illuminate the already bright and warm interior. While waiting for her turn, Auntie Jen whips out her trusted notebook. She had spent her weeks leading to this day reading and researching countless publications and websites. Her personal organizer – once filled with client appointments is now covered in rainbow highlights, post-its, scribbles and to read lists. Honestly, Auntie Jen could not even recall when was the last time she studied so hard.
“Was it my Final Year in Law School?”
CT-Simulation

“Jennifer Renée Lee”
Her name being announced over the PA system somewhat startled her.
“Alright. I can do this.”
As Auntie Jen got up from her seat, she was greeted by a young and friendly personnel who introduced herself as the Radiation Therapist in charge of her CT-simulation procedure today.
Before being ushered into the room with the CT-scanner, the Radiation Therapist double-checks her patient ID and goes through a quick checklist to give her an overview of what is to be expected during the procedure.
The checklist looks something like this:
- Patient Name and ID
- Contrast & Allergies
- Immobilization Devices
- Scanning Procedure
- Body Landmarks (i.e. Tattoos)
The steps were clearly explained and concise but Auntie Jen had some additional questions to what “immobilization and tattoos” were used for.
“We will be using customized immobilization devices like a form-fitting body mould (also known as a vacuum bag) that helps to maintain your body’s position the same way on a day to day basis. Tattoos on the other hand, are actually tiny, little permanent dots that will demarcate your treatment area in order to help the team direct the radiation treatment properly each day.”
“The whole process should not take longer than an hour.”
Example of a CT-Simulation process whereby a body mould (vacuum bag) is fabricated and how a tattoo is made (view at your own discretion)
Video credit: Nicole Young, YouTube (2013)
True enough, after about an hour, Auntie Jen is changing out of her patient gown and into the casual outfit she arrived in. The Radiation Therapist informs Auntie Jen that the treatment team will be calling her again to schedule her treatment appointment in about 1 – 2 weeks’ time. This is because the next step in the Radiation Therapy process will be Treatment Planning.
Treatment Planning
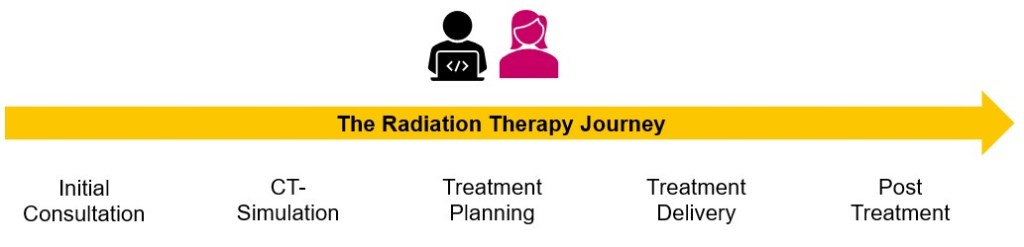
This step involves the Radiation Oncologist and the Medical Physicist4 (a professional who uses complex planning software to create treatment plans and performs quality assurance procedures for the linear accelerators) who will carefully create the radiation treatment plans using the CT scan images of Auntie Jen acquired during CT-simulation.
The focus of the treatment planning process is to deliver a high dose of radiation to the cancer while sparing the surrounding normal tissues. This helps preserve normal tissue and reduces the side effects of treatment. Treatment plans are curated using sophisticated treatment planning systems and are customized for each patient – therefore being the blueprint for treatment delivery.3

Source: https://en.wikipedia.org/wiki/Radiation_treatment_planning
Auntie Jen breathes a sigh of relief as she steps out of the Cancer Centre. The dark cloud that hung over her head earlier today had subsided and she now felt more confident and prepared for what is to come.
Treatment Delivery

Just over a week from the CT-simulation procedure, Auntie Jen receives another call from the Radiation Oncology department for her first day of treatment.
In contrast to the anxiety that she felt during her first trip to the Cancer Centre, this time, Auntie Jen feels more determined and hopeful. Mostly because she feels that the team made sure to help her understand each step in the Radiation Therapy process and also gave her room to ask questions whenever she had any. At every checkpoint, Auntie Jen felt supported and informed.
The treatment team of Radiation Therapists had prepped Auntie Jen mentally by verbally taking her through the treatment delivery steps. They also provided some snapshots of the treatment room, and briefed Auntie Jen of the precautions she’d need to be aware of when the radiation beam is being delivered.

(Author’s Note: The bunny at the foot of the treatment couch was gifted to me by my then-Manager)
As Auntie Jen walks into the treatment room, she feels the icy chills from the air-conditioning against her skin; but the soft jazz music playing in the background and the friendly smiles from the therapists makes her feel a whole lot warmer.
“Looks like this is going to be “home” for the next 28 times of radiation treatment.”
Before Auntie Jen got onto the treatment couch, she couldn’t help but gaze in awe at the technological marvel standing in front of her. The sheer size of the linear accelerator machine that would be delivering her radiation treatment over the course of just under 6 weeks can be quite intimidating.
As she lay down on her back on the treatment couch, the therapists begin positioning Auntie Jen using the same immobilization devices that were used during the CT-simulation process. After which, careful physical adjustments were made to ensure that the little tattoos made prior were also corresponding to the lasers used as reference.
Once the therapists were happy with Auntie Jen’s initial treatment position, they remind her that the machine will be rotating around and about; and for her to not be alarmed by the humming sound from the machine as it delivers radiation.
They reassure her that the entire procedure will be painless and that the team will be monitoring her in real-time via CCTVs. Auntie Jen will also be able to communicate with them via the in-room intercom and vice versa.
Before leaving the room, one of the therapists glances over at Auntie Jen and gives her a reassuring look.
“Don’t worry Ma’am. Just keep still and this process will not take longer than 20 minutes. We will see you real soon.”
Example of the Treatment Positioning and Delivery process. This process may slightly differ depending on the area to be treated.
Video Credit: RANZCR, YouTube (2014)
Before she knew it, the therapists were back in the room again to help Auntie Jen get off the treatment couch.
“That’s it for today, Ma’am. Great job on Day 1! Before you leave, Nurse Sasha here will take you to the adjacent room to quickly brief you on radiation treatment care. However, we will be seeing you again tomorrow – same time, same place.”
Nurse Sasha is a Radiation Oncology Nurse1 (a nurse that specializes in caring for people receiving radiation therapy) and she her role is to help Auntie Jen understand the steps to care for her radiation treatment area. In this scenario, as Auntie Jen is receiving treatment to her pelvis, Nurse Sasha advises her of the common side effects pertaining to this area, in addition to skin care and nutrition during treatment.
As Auntie Jen got into her car, she let out a long sigh of relief, “Day 1 – checked!”

Post Treatment Follow-up
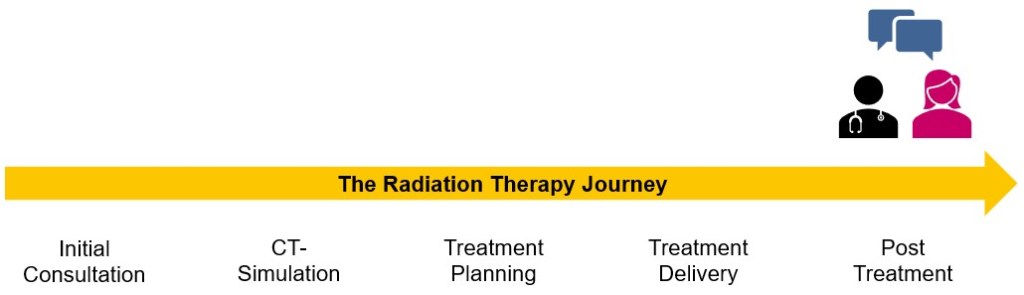
Once the course of radiation treatment is complete, a follow-up appointment will be given to the patient in order to monitor their recovery and overall status. Initially, this follow-up procedure could be once at every quarter of the year; and as time goes by, the frequency of these visits will decrease. While cancer may be the start of an ongoing conversation with doctors and healthcare professionals, the conclusion of treatment rarely spells the end of that conversation. Most patients usually continue this form of support until the end of their days.
The most important thing in communication is to hear what isn’t being said.
– Peter Drucker
References:
1. Cancer.Net. (2020, September 23). What to Expect When Having Radiation Therapy. https://www.cancer.net/navigating-cancer-care/how-cancer-treated/radiation-therapy/what-expect-when-having-radiation-therapy
2. Health Times. (2021, April 26). What does a Radiation Therapist do? https://healthtimes.com.au/hub/oncology/4/guidance/nc1/what-does-a-radiation-therapist-do/553/
3. Stony Brook Cancer Center. (2020). Radiation Therapy Process | Stony Brook Cancer Center. Radiation Oncology. https://cancer.stonybrookmedicine.edu/RadiationTherapyProcess
4. IOMP (2020). Medical Physics – International Organization for Medical Physics. https://www.iomp.org/medical-physics/
5. Background audio credit: Bensound.com

It brought back old memories as I was reading through this write up.
Thank you God for the 2nd chance!
LikeLike